In modern medicine, anticoagulants play a crucial role in preventing and treating thrombotic diseases. Among them, the novel oral anticoagulant apixaban has gradually become a clinical focus due to its unique mechanism of action and advantages. So what exactly is apixaban? What are its characteristics and uses? Let's explore in depth.
I. Understanding Apixaban
-
What is apixaban?
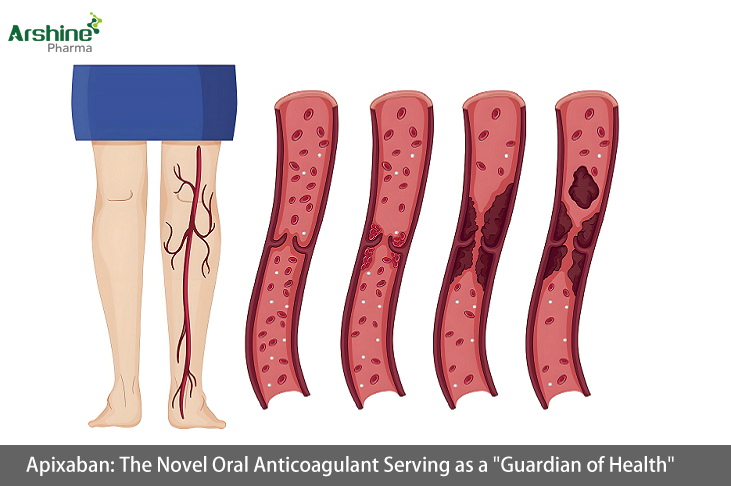
Apixaban is a novel oral anticoagulant that directly, reversibly, and highly selectively blocks the active site of factor Xa, thereby inhibiting the conversion of prothrombin to thrombin and effectively preventing thrombus formation. Compared to rivaroxaban, apixaban not only directly inhibits factor Xa but also exerts anticoagulant effects by indirectly inhibiting thrombin-induced platelet aggregation and reducing thrombin production. Apixaban was first approved in the EU in 2011, in Japan in 2012, and in China in 2013. It was included in China's National Reimbursement Drug List in 2017. -
Specifications and indications
Apixaban is available in 2.5mg tablets. In China, it is mainly indicated for adult patients undergoing elective hip or knee replacement surgery to prevent venous thromboembolic events. The U.S. FDA has approved broader indications, including reducing the risk of stroke and systemic embolism in patients with non-valvular atrial fibrillation, reducing the recurrence of deep vein thrombosis and pulmonary embolism, and treating deep vein thrombosis and pulmonary embolism.
II. Administration of Apixaban
-
Dosage and administration
For adult patients undergoing elective hip or knee replacement surgery to prevent venous thromboembolic events, the recommended dose is 2.5mg twice daily, taken orally with water, regardless of meals. The first dose should be administered 12-24 hours after surgery. Physicians should determine the exact timing within this window by weighing the potential benefits of early anticoagulation against postoperative bleeding risks. The treatment duration is 32-38 days after hip replacement and 10-14 days after knee replacement. -
Missed dose
If a dose is missed, the patient should take it immediately and then continue with twice-daily dosing. When switching from injectable anticoagulants to apixaban, the first dose can be taken at the next scheduled time, and vice versa. -
Alternative administration methods
For patients who cannot swallow tablets whole, apixaban can be crushed and suspended in water, 5% glucose solution, or apple juice, or mixed with applesauce for immediate oral administration. It can also be crushed, suspended in 60mL of water or 5% glucose solution, and administered immediately via nasogastric tube. Crushed apixaban remains stable in water, 5% glucose, apple juice, or applesauce for up to 4 hours.
III. Adverse Reactions and Precautions
-
Adverse reactions
Common adverse reactions include anemia, bleeding, bruising, and nausea. Less common reactions (occurring in <1% of patients) include allergic reactions (e.g., rash, angioedema) and syncope. -
Bleeding risk
Monitor for signs of bleeding during treatment. Apixaban should be used cautiously in patients with bleeding risks, including congenital/acquired bleeding disorders, active gastrointestinal ulcers, bacterial endocarditis, thrombocytopenia, platelet dysfunction, history of hemorrhagic stroke, uncontrolled severe hypertension, or recent brain/spinal/eye surgery. Discontinue immediately if severe bleeding occurs. -
Temporary discontinuation risk
Discontinuing anticoagulants during active bleeding, elective surgery, or invasive procedures increases thrombotic risk. If apixaban must be temporarily stopped, restart anticoagulation as soon as possible.
IV. Special Populations
-
Pregnant/lactating women
No data exist on apixaban use during pregnancy; it is not recommended. It is unknown whether apixaban or metabolites are excreted in human milk, but animal studies show excretion in milk, so risks to newborns/infants cannot be excluded. Either discontinue breastfeeding or avoid apixaban therapy. -
Pediatric patients
No safety or efficacy data are available for patients under 18 years. -
Elderly patients
No dose adjustment is needed. -
Renal impairment
(1) No adjustment for CrCl ≥30 mL/(min·1.73m²);
(2) Use cautiously for CrCl 15-29 mL/(min·1.73m²) due to elevated plasma levels and bleeding risk. Recommended dose for VTE: 2.5mg twice daily;
(3) For dialysis patients with CrCl <15 mL/(min·1.73m²) and VTE: 2.5mg twice daily;
(4) Contraindicated in non-dialysis patients with CrCl <15 mL/(min·1.73m²). -
Hepatic impairment
Contraindicated in patients with coagulopathy and clinically significant bleeding risk. Not recommended in severe impairment. No dose adjustment for mild impairment. No recommendations exist for moderate impairment.
V. Drug Interactions
-
Increased effect/bleeding risk
(1) Avoid concomitant use with CYP3A4/P-gp inhibitors (e.g., azole antifungals like ketoconazole/itraconazole/posaconazole; HIV protease inhibitors like ritonavir);
(2) Use NSAIDs (naproxen, aspirin) or antiplatelets (clopidogrel) cautiously. -
Decreased effect/thrombosis risk
Avoid CYP3A4/P-gp inducers (e.g., rifampin, phenytoin, phenobarbital, St. John’s wort, carbamazepine).
In summary, as a novel oral anticoagulant, apixaban plays an important role in preventing and treating thrombotic diseases. However, strict adherence to medical advice is essential, including monitoring adverse reactions, special population considerations, and avoiding drug interactions to ensure safe and effective use.
